Our Research Pursuits
Our department consists of several research teams with several multidisciplinary affiliations, which focus both on basic and clinical and translational research. Our basic research teams are primarily located in the beautiful, state-of the-art Health Sciences Research Facility III. Our department is recognized nationally as one of the top-tier, well-funded Otolaryngology research departments. Among our areas of research expertise are genetic hearing loss, epigenetic alterations associated with malignancy, and tumor immunology. Our labs work in close proximity and hold joint lab meetings and journal clubs to promote collaborative endeavors. Additionally, the Department has established strong alliances with basic science departments, such as Biochemistry, Microbiology, Institute of Genome Sciences, and Program for Personalized and Genomic Medicine, to create a multi-disciplinary network that enhances translational research pursuits.

The team of Dr. Ahmed is focused on understanding how the retinal and inner ear sensory epithelia develop and function. Dr. Ahmed’s research interests consist of: (1) Inherited human disorders of retina and inner ear, like Usher syndrome (USH); and (2) Oculocutaneous Albinism (OCA). The studies under investigation are designed to answer the following broad questions: What are the precise mechanisms of various forms of hearing and vision dysfunction? What are the genetic factors that determine light sensitivity? How do the pathogenic mutations in disease-causing genes affect the ear, eye and skin structure and function? And which molecules or genetic factors can exacerbate and/or mitigate the effects of disease-causing genes? For these studies, families segregating inherited USH and OCA are being collected. Mutant mouse and zebrafish models have been developed and we evaluate them to understand the function of new proteins. Functional analysis of the newly identified genes associated with deaf-blindness and OCA promises new insights into the molecular mechanisms of vision and auditory development and functions and will facilitate the rational design of potential therapies.

Dr. Riazuddin’s team is focused on understanding the molecular and genetic basis of hearing impairment. This is done by ascertaining large human families segregating hearing loss and through genetic screening; disease causing mutations are identified in these families. The identified mutations are further studied by analyzing the orthologous mutant mouse models, which are evaluated for developmental, structural and physiological defects of the inner ear. This will help us better understand the mutated genes and the underlying molecular mechanism of the hearing process. Identification of such genes will help in early and more accurate diagnosis for certain forms of hereditary hear impairments. The lab uses various approaches ranging from genetic analysis of human DNA samples to screen and identify the candidate genes, to molecular biological approaches to determine the expression of gene under study at protein /RNA level. To further study the target genes different model systems are exploited which include but are not limited to mouse, Zebrafish etc, where expression, localization and morphology of the inner ear is compared to wild type controls.

Dr. Hertzano’s research laboratory uses cell type-specific approaches to (1) define the key regulatory events that lead to cell type-specific differentiation. Specifically, identification and characterization of transcriptional cascades that lead to hair cell terminal differentiation and survival as a crucial step in developing regenerative treatments for hearing loss; and (2) defining the molecular events as a result of acquired and noise-induced hearing loss to develop novel approaches for prevention and treatment of these problems. The team uses cell type-specific genomic approaches in mice and zebrafish, followed by validation using genetically engineered animal models and classic experimental and developmental biology techniques.

Dr Isaiah’s research interests span the domains of (i) innovative analytic tools, (ii) children’s brain development and neurocognitive outcomes, and (iii) biomedical device development. His group uses advanced statistical models, visualization techniques and machine learning to dissect long-held associations and causal conclusions within large heterogeneous datasets with application to children’s health. Of interest is the domain of pediatric sleep disordered breathing, where he has published extensively on the use of causal mediation models to better identify the extent of the relationship between the severity of upper airway obstruction on neurobehavioral outcomes. He is closely involved in the Adolescent Brain Cognitive Development Study, the largest study of brain development in children, in which he studies the impact of the environmental stressors on brain development. Lastly, he continues to develop, in collaboration with scientists at the University of Maryland, College Park, medical technologies specifically with application to children’s health and respiratory sensing.
Adam C. Kaufman, MD, PhD
Assistant Professor

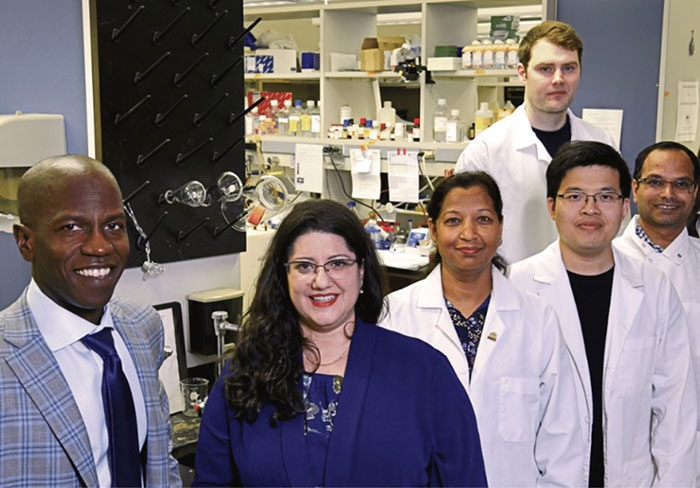
Dr. Daria Gaykalova heads the translational laboratory, which defines the functional role of epigenetics in transcriptional regulation of cancer development and progression, mutational burden, and immunological landscape in tumors. The goal of her lab is to define the tumor-type-specific epigenetic treatment, especially for tumors that don’t have any disease-specific treatment protocols, such as HPV-related head and neck squamous cell carcinoma (HPV+ HNSCC). Her recent studies suggest that the chromatin landscape is the primary driver of viral integration, cancer-specific gene expression, and alternative splicing landscape in HNSCC. These data indicate that the combination of epigenetic treatment with the inhibitors of oncogenic and alternative protein expression is especially potent for cancer treatment. Her group adopted diverse high-throughput analyses for various preclinical models and primary patient samples, bridging high-throughput data analysis, robust experimental validation, and drug treatment. The research is funded by multiple sources, including NIH awards.
Dr. Taylor is a surgeon-scientist whose clinical practice is dedicated to the comprehensive care of patients with head and neck pathology. He has established an academic-tertiary practice with patients referred for complex surgical management of head and neck malignancy, skull base tumors, thyroid cancer and parathyroid tumors, and sino-nasal disease. His research goals are aligned with his clinical objectives: to improve the survival of patients with head and neck cancer. His lab has focused on factors impacting immune-cytotoxicity and immune-tolerance. His lab has extensive experience working with squamous cell cancer of the head and neck (SCCHN) cell lines and murine xenograft tumor models. Based upon findings from his laboratory, he initiated and completed a multi-institutional clinical trial evaluating the impact of NK FcγRIIIa polymorphisms on antibody-based therapy for SCCHN. This work has provided insight into which patients best benefit from antibody-based therapy for SCCHN. His lab currently has forged a collaboration with Dr. Zalzman’s lab and he has successfully established murine models to study head and neck cancer stem cell immortality mechanisms using xenografts. Additionally, the two labs have combined to harvest adult mesenchymal stem cells to both improve their long-term survival in culture while preserving their differentiation potential ultimately facilitating advancements for regenerative medicine .

Dr. Michal Zalzman is a molecular cell biologist and a stem-cells expert who made significant discoveries related to a novel mechanism triggered by ZSCAN4, controlling replicative lifespan of embryonic stem cells. Her studies are published in leading journals such as Nature, Cell Stem Cells, Stem Cell Research and Therapy, Oncogene and PNAS. Using the technology developed in the Zalzman laboratory, her team establishes novel protocols for 3D-printed adult-stem cell implants for regenerative medicine and bone reconstructive surgeries. Further, the team develops novel stem cell therapies for neurodegenerative diseases. In collaboration with Dr. Rodney Taylor, her laboratory further studies the human ZSCAN4 mechanism components and function, with the goal to develop these targets as new strategies for cancer precision medicine. Dr. Zalzman and her team holds multiple patents and patent applications based on her work, and her research is funded by major federal grant awards from NIAMS and NINDS/National Institutes of Health.

Dr. Schulze is currently developing a molecular approach that can be used in treatment of tumors using a novel Chimeric Antigen Receptors (CARs) system. CARs routinely contain a binding domain and a T cell activation domain. Most CARs are engineered with a very specific antibody binding domain to target the cancer cells and this domain is fused to the T cell activation domain to treat cancers. Our novel receptor has an Fc receptor binding domain that binds to all antibodies. Treatment is based on the specific anti-cancer antibodies given to the patient. For example, injected antibodies bind to the Fc receptor resulting in activation of the patients own T cells which can kill the cancer cells. We are developing this novel CAR receptor that can be used to target tumors of the Head and Neck. This CAR system is an improvement over existing CARs in that 1) a single construct can be used for all patients, 2) specificity of treatment depends on the antibodies administered 3) combinational antibody treatment can be given to improve killing of the cancer and 4) if a specific antibody loses effectiveness and different antibody can be administered. This approach of a “universal binding CAR” can potentially be used with antibodies for improved treatment of Head and Neck tumors.
