February 26, 2025 | Katie Ghiardi
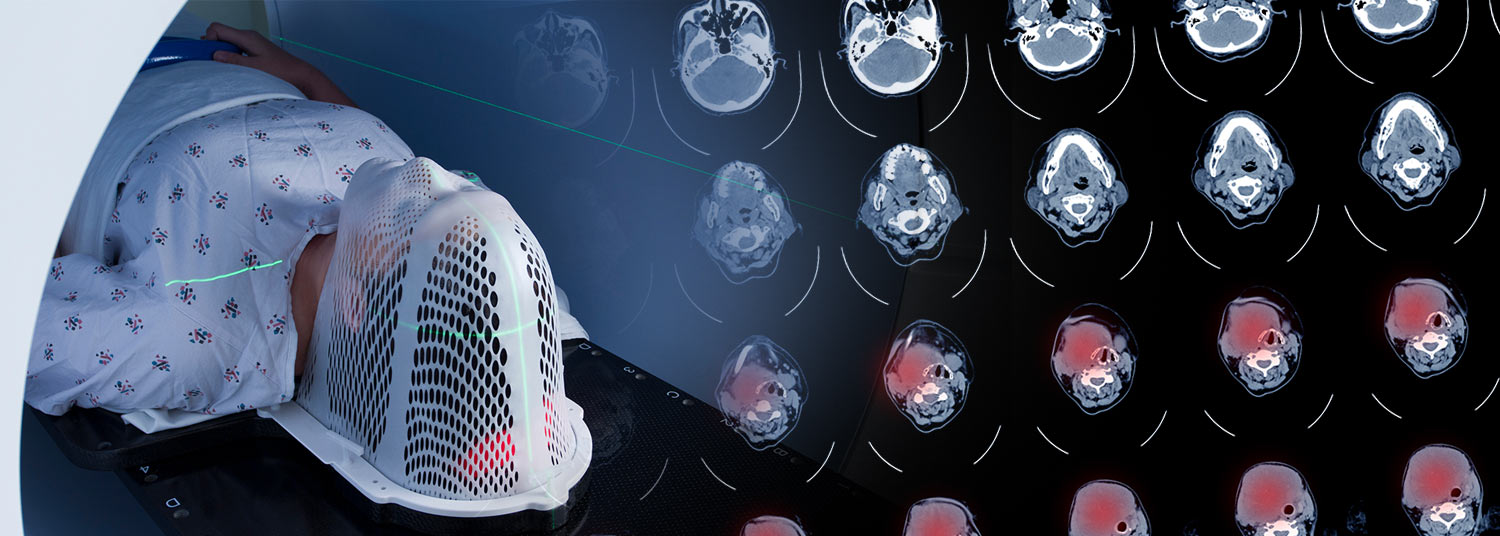
Data collected in pre-treatment CT-scans may provide important imaging biomarkers to better predict patient prognosis, and potentially customize treatment strategies
Cancers occurring in the mouth, nose, and throat are on the rise in the U.S., especially in younger people. About 60,000 new cases are diagnosed every year with one in five cases occurring in people younger than 55, according to the American Cancer Society. A new study provides insights that may eventually help oncologists better predict how the disease will respond to certain therapies, leading to improved survival outcomes for patients.
 The findings were recently published in the journal Scientific Reports. A team of researchers from the University of Maryland School of Medicine (UMSOM) Department of Radiation Oncology and the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC) analyzed the pre-treatment CT scans of patients with head and neck squamous cell carcinoma (HNSCC) to locate radiomic biomarkers that can be used to predict the aggressiveness of the disease and its response to treatment.
The findings were recently published in the journal Scientific Reports. A team of researchers from the University of Maryland School of Medicine (UMSOM) Department of Radiation Oncology and the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC) analyzed the pre-treatment CT scans of patients with head and neck squamous cell carcinoma (HNSCC) to locate radiomic biomarkers that can be used to predict the aggressiveness of the disease and its response to treatment.
CT scans are a standard pre-treatment diagnostic tool for patients with HNSCC and are used by oncologists to create individualized treatment plans. In this study, researchers took a closer look at the data collected by these scans in 203 patients from UMGCCC and 77 patients from the MD Anderson Cancer Center dating back to 2003. Using radiomics, advanced mathematical and statistical algorithms, they identified tumor features that are not otherwise visible to the human eye. These biomarkers were then used to develop predictive models for treatment, focusing on the likelihood of progression-free survival after treatment. Researchers concluded that the identification of these radiomic biomarkers offer valuable insights into who will be most likely to benefit from certain treatments.
“Integrating prognostic and predictive biomarkers into clinical care could help to provide more targeted therapies, leading to improved survival outcomes for patients,” said the study’s Senior Author, Lei Ren, PhD, Professor of Radiation Oncology and Associate Chief of Physics Research in the Department of Radiation Oncology at UMSOM. “The findings from this study pave the way for future investigations through larger clinical trials to further evaluate the clinical efficacy of radiomics biomarkers for progression-free survival prediction in HNSCC patients.”
 Despite advancements in surgical techniques and other therapies, the 5-year survival rate for HNSCC remains around 50 percent. Tobacco smoking and alcohol consumption significantly increase the risk of HNSCC, as well as certain strains of Human Papillomavirus (HPV).
Despite advancements in surgical techniques and other therapies, the 5-year survival rate for HNSCC remains around 50 percent. Tobacco smoking and alcohol consumption significantly increase the risk of HNSCC, as well as certain strains of Human Papillomavirus (HPV).
Typical treatment for these cancers may include surgically removing the tumor, administering radiation to the affected area, or giving the patient a regimen of chemotherapy, immunotherapy, or a combination of therapies. These treatments can cause potentially permanent side effects impacting a patient’s ability to see, swallow, or speak. Researchers found that the use of radiomic biomarkers in treatment planning may also allow oncologists to recommend less invasive treatment protocols, therefore reducing the risk of lasting side effects.
 “This research is reflective of our goal at UMGCCC to improve outcomes and reduce side effects for patients with HNSCC and other forms of cancer,” said William F. Regine, MD, the Isadore and Fannie Schneider Foxman Professor and Chair of the University of Maryland Department of Radiation Oncology. “Exacting imaging biomarkers from standard-of-care CT scans offers a noninvasive approach without additional costs to patients.”
“This research is reflective of our goal at UMGCCC to improve outcomes and reduce side effects for patients with HNSCC and other forms of cancer,” said William F. Regine, MD, the Isadore and Fannie Schneider Foxman Professor and Chair of the University of Maryland Department of Radiation Oncology. “Exacting imaging biomarkers from standard-of-care CT scans offers a noninvasive approach without additional costs to patients.”
“Our Institute for Genome Sciences team played a crucial role in this study by helping to acquire the clinical data necessary for analysis, as well as evaluating and validating the obtained results,” said Daria Gaykalova, PhD, Associate Professor of Otorhinolaryngology at UMSOM and researcher at IGS. “We are proud to contribute to research in head and neck and other forms of cancer to learn more about causes and treatments.”
 In future studies, researchers hope to gain a better understanding of these imaging biomarkers and their underlying meaning and validate their findings in data from other institutions. This research will need to be completed before a prospective clinical trial could be offered to patients for treatment intervention based on the imaging biomarkers and prognosis prediction. For example, patients with imaging biomarkers associated with less aggressive disease might be offered a decreased radiation protocol.
In future studies, researchers hope to gain a better understanding of these imaging biomarkers and their underlying meaning and validate their findings in data from other institutions. This research will need to be completed before a prospective clinical trial could be offered to patients for treatment intervention based on the imaging biomarkers and prognosis prediction. For example, patients with imaging biomarkers associated with less aggressive disease might be offered a decreased radiation protocol.
“While preliminary, this study offers a promising path forward to learn about novel predictors of response and to develop a non-invasive tool to personalize different treatment options for head and neck cancers,” said Taofeek K. Owonikoko, MD, PhD, Executive Director of UMGCCC and the Marlene and Stewart Greenebaum Distinguished Professor of Oncology at UMSOM.
The study was funded in part by the National Institutes of Health (NIH) grants R01DE033426and U54CA273956, and the National Institute of Dental and Craniofacial Research (NIDCR). NIDCR’s stated mission is to improve oral, dental, and craniofacial health through research, research training, and the dissemination of health information.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System ("University of Maryland Medicine") has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2023, the UM School of Medicine is ranked #10 among the 92 public medical schools in the U.S., and in the top 16 percent (#32) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
About the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center
The University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center is a National Cancer Institute-designated comprehensive cancer center within the University of Maryland Medical Center in Baltimore, the flagship academic hospital of the
University of Maryland Medical System. It offers a multidisciplinary approach to treating all types of cancer and has an active clinical and basic science research program through its relationship with the University of Maryland School of Medicine. The center is ranked among the top 50 cancer programs in the country by US News & World Report. www.umgccc.org
Contact
Katie Ghiardi
Lead Media & Public Relations Specialist
University of Maryland Marlene and Stewart Greenebaum
Comprehensive Cancer Center
KGhiardi@som.umaryland.edu
Related stories

Wednesday, April 09, 2025
Unite for Hope: Maryland Half Marathon & 5K Calls on Runners and Walkers to Fuel Cancer Research
Marking its 17th year, the Maryland Half Marathon & 5K returns to the Maple Lawn community in Howard County on Saturday, June 7, 2025. This signature event empowers runners, walkers, and fundraisers to join forces against cancer, driving critical support for the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC). Since 2009, the Maryland Half Marathon & 5K has raised over $6 million, fueling groundbreaking research and compassionate patient care.

Wednesday, December 04, 2024
Business Leader and Philanthropist Michael Greenebaum Named New Chair of the University of Maryland School of Medicine's Board of Visitors
University of Maryland School of Medicine (UMSOM) Dean Mark T. Gladwin, MD, has announced that prominent business leader and philanthropist Michael Greenebaum has been named Chair of the School's Board of Visitors. Mr. Greenebaum served as the Inaugural Vice Chair of the Board of Visitors since 2021 and has been a board member since 2012.

Monday, May 08, 2023
Patients with Advanced Prostate Cancer May Benefit from Focused Radiation Therapy that Targets Metastases
University of Maryland School of Medicine (UMSOM) faculty recently launched a new clinical trial to test a targeted form of highly-focused radiation therapy in patients with advanced prostate cancer that has spread to distant sites in the body. The study aims to determine whether the innovative approach – which uses highly-focused radiation beams to carefully target small metastases – can extend survival in these patients.

Thursday, March 09, 2023
Leading Physician-Scientist Dr. William F. Regine Named Senior Associate Dean for Clinical Affairs at UM School of Medicine and President of UM Faculty Physicians, Inc.
University of Maryland School of Medicine (UMSOM) Dean Mark T. Gladwin, MD announced today that William F. Regine, MD, FACR, FASTRO, FACRO has been appointed to the executive role of Senior Associate Dean for Clinical Affairs at the University of Maryland School of Medicine (SOM), effective immediately.

Tuesday, December 07, 2021
UM School of Medicine's Department of Radiation Oncology Announces that Preeminent Scientist, Dr. Zeljko Vujaskovic, will Transition to New Role in the Department
University of Maryland School of Medicine (UMSOM) Radiation Oncology Department Chair William F. Regine, MD, FACR, FACRO, announced today that Zeljko Vujaskovic, MD, PhD, Professor and Vice Chair for Research in the Department of Radiation Oncology, will transition from his current faculty position to a new role in the Department, effective December 3, 2021.

Thursday, July 15, 2021
University of Maryland Greenebaum Comprehensive Cancer Center Earns Renewal of Highest Designation for Cancer Center Excellence from National Cancer Institute
The University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC) has earned renewal of its National Cancer Institute (NCI) designation as a Comprehensive Cancer Center for another five years. The prestigious distinction recognizes the cancer center’s high caliber of scientific leadership and robust programs in basic, clinical and population science research, placing it in the top echelon of cancer centers nationwide.
Friday, July 26, 2019
Dr. Amit Sawant Named Chief of Division of Medical Physics in Radiation Oncology
William F. Regine, MD, FACRO, the Isadore and Fannie Schneider Foxman Chair and Professor of Radiation Oncology at the University of Maryland School of Medicine (UMSOM), and Dean E. Albert Reece, MD, PhD, MBA, announced today that Amit Sawant, PhD, MS, Associate Professor of Radiation Oncology, has been named Chief of Medical Physics in the Department of Radiation Oncology.