July 24, 2023 | Vanessa McMains
Opioids remain the most potent and effective pain relievers in medicine, but they’re also among the most addictive drugs that can halt a person’s ability to breathe during an overdose — which can be deadly. Researchers have been racing to develop safer pain reliever drugs that target a specific opioid receptor, called the kappa opioid receptor, that is only found in the central nervous system and not elsewhere in the body, like other opioid receptors. Previous research suggests that such drugs may not lead to addiction or death due to overdose, but the currently known drugs that target these kappa opioid receptors have their own set of unacceptable side effects, including depression and psychosis.
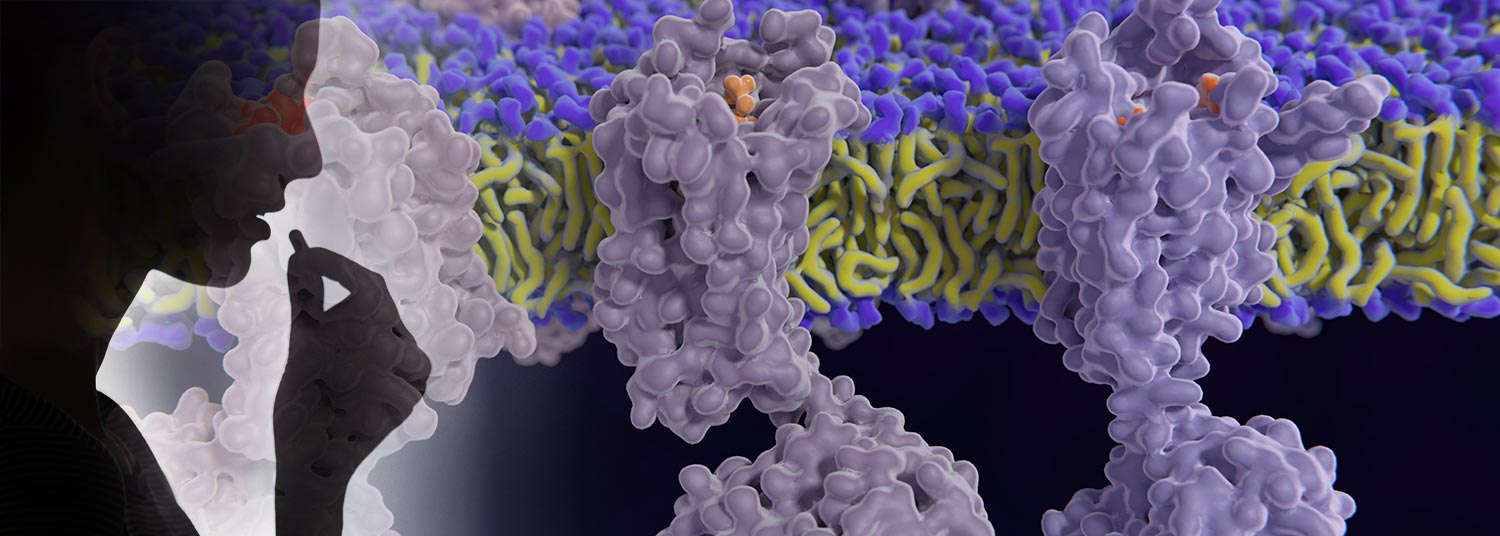
In one of the first steps towards eventually developing a new wave of kappa opioid receptor drugs without these side effects, researchers at the University of Maryland School of Medicine and Washington University have mapped the 3D structure of the central nervous system specific kappa opioid receptor and figured out how it differs from the other opioid receptors. In this new study, they discovered what instructs the kappa opioid receptor to change its shape, which uniquely binds to opioid drugs, akin to a lock fitting with a specific key.
They published their results in the May issue of Nature.
 Aside from relieving pain, opioid receptors are also involved in everything from sensing taste and smell to digestion and breathing, as well as responding to many of the body’s hormones. The way that opioid receptors can influence so many functions around the body is by acting with one of seven cell activity proteins, known as G-alpha proteins, that each help to specialize the function they suppress in the cell.
Aside from relieving pain, opioid receptors are also involved in everything from sensing taste and smell to digestion and breathing, as well as responding to many of the body’s hormones. The way that opioid receptors can influence so many functions around the body is by acting with one of seven cell activity proteins, known as G-alpha proteins, that each help to specialize the function they suppress in the cell.
“Knowing how these drugs interact with opioid receptors and having a clear view of this molecular snapshot is critical for allowing researchers to develop more effective pain-relieving drugs. This requires a drug that binds to the right type of opioid receptor, such as one in the central nervous system to reduce pain versus the ones that interact in the gut, causing side effects like constipation,” said study corresponding author Jonathan Fay, PhD, Assistant Professor of Biochemistry and Molecular Biology at UMSOM. “Additionally, these next generation medications will need to be designed with the appropriate kind of G-alpha protein in mind, as this will help to precisely target location and cell function by determining the specific shape of the opioid receptor — so the drug only reduces pain without affecting other body functions.”
The known kappa opioid receptor drugs do not produce the same euphoria as traditional opioid drugs, making these kappa opioid receptor drugs less likely to be addictive.
For the current study, the researchers used cryogenic electron microscopy in order to visualize the structure of the kappa opioid receptor. They first needed to flash freeze the receptors, which were bound to a hallucinogenic drug with one of two of the traditional G-alpha proteins. They then used a different drug to see how the kappa opioid receptor interacted with two other types of G-alpha proteins; one of these G-alpha proteins is found only in the central nervous system and the other is used to detect taste and smell.
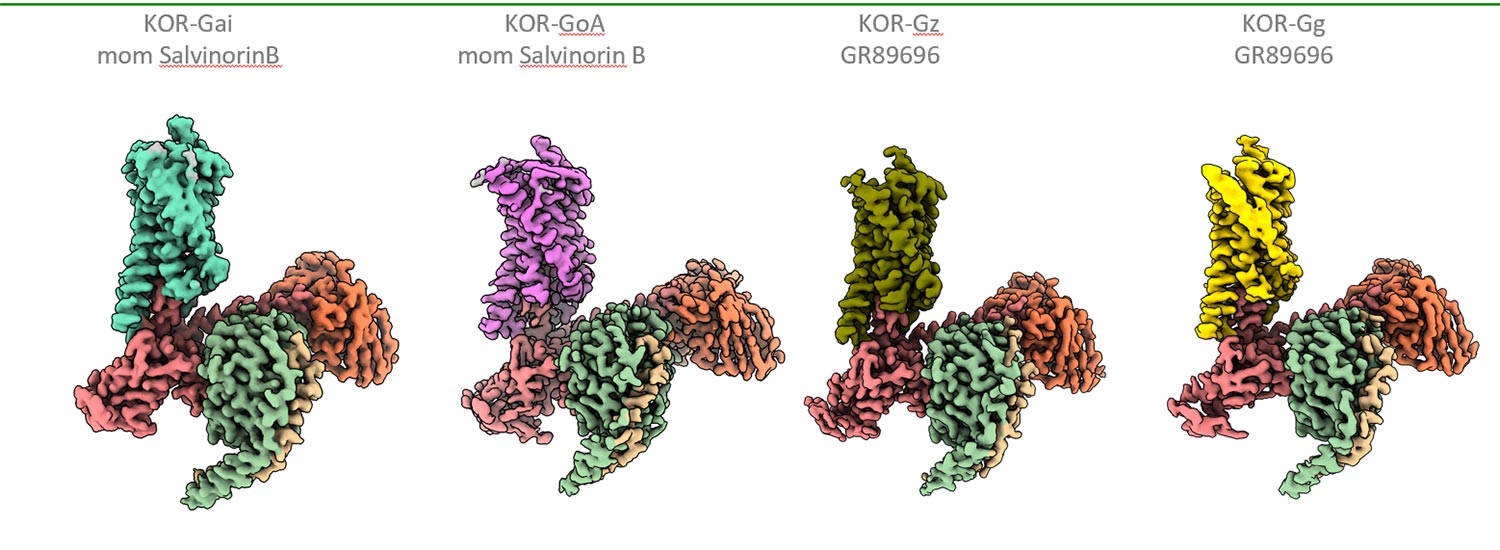
Dr. Fay described the G-protein as shaped like a chainsaw with a handle and a ripcord. Each G-protein had a slightly different position of its chainsaw handle when bound to the kappa opioid receptor. This change in position played an active role in determining the shape of the kappa opioid receptor and thus what drug bound the best to it. These findings ultimately could have implications for how new drugs will be designed.
 UMSOM Dean Mark T. Gladwin, MD, Vice President for Medical Affairs, University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor, said, “Researchers face an enormous challenge in developing safer pain-reliever drugs since they will need to target both the correct opioid receptor as well as the appropriate G-alpha protein. Studies like these reinforce the mission of our new Kahlert Institute for Addiction Medicine, which aims to help develop this next generation of engineered small molecule drugs that are less addictive.
UMSOM Dean Mark T. Gladwin, MD, Vice President for Medical Affairs, University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor, said, “Researchers face an enormous challenge in developing safer pain-reliever drugs since they will need to target both the correct opioid receptor as well as the appropriate G-alpha protein. Studies like these reinforce the mission of our new Kahlert Institute for Addiction Medicine, which aims to help develop this next generation of engineered small molecule drugs that are less addictive.
The research was supported by National Institutes of Health grants from the National Institute of General Medical Sciences (R35GM143061) and the National Institute of Neurological Disorders and Stroke (R01NS099341). The Titan X Pascal graphics card used for this research was donated by NVIDIA.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world — with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic, and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Deborah Kotz
Senior Director of Media Relations
Office of Public Affairs & Communications
University of Maryland School of Medicine
Email: DKotz@som.umaryland.edu
o: 410-706-4255
c: 410-804-0054
t: @debkotz2
Related stories

Tuesday, December 09, 2025
University of Maryland School of Medicine Names Distinguished Scientist and Academic Leader Gerald M. Wilson, PhD, as Chair of the Department of Biochemistry and Molecular Biology
University of Maryland School of Medicine (UMSOM) Dean Mark T. Gladwin, MD today announced the appointment of Gerald M. Wilson, PhD, as Chair of the School’s Department of Biochemistry and Molecular Biology, effective December 15, 2025. Dr. Wilson, a distinguished scientist and educator, brings more than two decades of leadership and internationally recognized research in RNA biochemistry and cancer mechanisms to this role. As part of the appointment, he will be endowed as the John F.B. Weaver Professor in Biochemistry and Molecular Biology.

Friday, December 15, 2023
UMSOM Researchers Discover First Ever Link Between Hemoglobin-Like Protein and Normal Cardiac Development
In a landmark study led by the University of Maryland School of Medicine, researchers discovered for the first time that a certain kind of protein similar to hemoglobin, called cytoglobin, plays an important role in the development of the heart. Specifically, it affects the correct left-right pattern of the heart and other asymmetric organs. The findings, published today in the journal Nature Communications, could eventually lead to the development of new therapeutic interventions to alter the processes that lead to these defects.
Friday, December 08, 2023
UM School of Medicine Mourns the Loss of Dynamic Researcher, Chair, World Traveler, Giuseppe Inesi, MD
The University of Maryland School of Medicine mourns the loss of a dynamic researcher and teacher, Giuseppe Inesi, MD. He passed away on November 12 in Tiburon, California of Alzheimer’s disease.
Friday, February 17, 2023
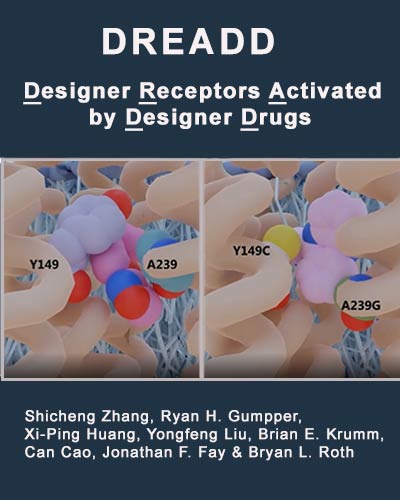
Neuroscience Tool’s Structure May Lead to Next Gen Versions
In order to more fully understand how diseases arise in the brain, scientists must unravel the intricate way neurons relay messages (either chemical or electrical) along a complex web of nerve cells. One way is by using a tool called DREADDs, which stands for Designer Receptors Activated by Designer Drugs. When introduced to a nerve cell or neuron, DREADDs acts like a specialized lock that only works when a key — in the form of a synthetic designer drug — fits into that lock. DREADDs can enable researchers to turn specific cell functions on or off to examine groups of neurons in circuits more precisely.

Thursday, April 16, 2020
University of Maryland School of Medicine Launches Center for Substance Use in Pregnancy
Asaf Keller, PhD, Professor and Interim Chair of the Department of Anatomy & Neurobiology at the University of Maryland School of Medicine (UMSOM), along with UMSOM Dean E. Albert Reece, MD, PhD, MBA, have announced the formation of a new research center to study the long-term health effects on the brains of children born to women who use drugs and alcohol during pregnancy. The Center for Substance Use in Pregnancy will conduct pre-clinical and clinical neuroscience research, focusing on the use of marijuana, opioids, nicotine and alcohol, all of which have increased dramatically in recent years.
