September 29, 2021 | Vanessa McMains
Findings suggest several FDA-approved drugs, such as a common diabetes medication and anesthetics, could protect from noise-related hearing loss.
A growing number of people suffer from hearing loss due to exposure to loud noises from heavy machinery, concerts, or explosions. As a result, scientists have been working to understand the mechanism behind how this damage to hearing actually occurs.
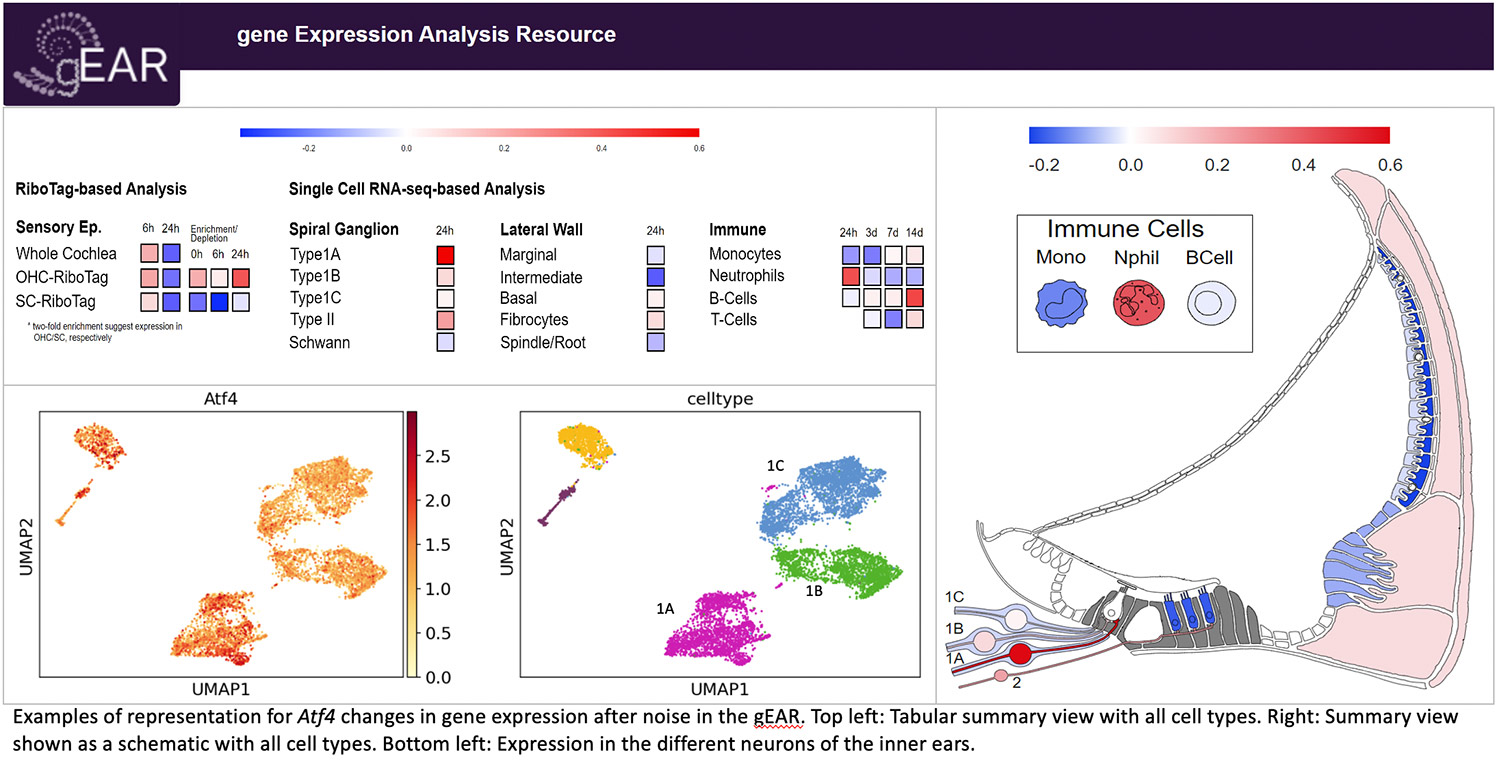
Now, a team led by researchers at the University of Maryland School of Medicine (UMSOM) has published an online interactive atlas representing the changes in the levels of RNA made in the different cell types in ears of mice, after damage due to loud noise. These changes in RNA levels are known as changes in “gene expression.”
Once they determined the larger trends in gene expression following the damage, the UMSOM scientists then searched a database of FDA-approved drugs to find those that are known to produce opposite patterns of those caused by the noise. From this analysis, the research teams identified a handful of drug candidates that may be able to prevent or treat the damage, and ultimately preserve hearing.
Their analysis was published in Cell Reports on September 28.
 “As an otolaryngologist surgeon-scientist, I see patients with hearing loss due to age or noise damage, and I want to be able to help prevent or even reverse the damage to their hearing,” said study leader Ronna Hertzano, MD, PhD, Professor of Otorhinolaryngology-Head & Neck Surgery, Anatomy and Neurobiology at UMSOM and Affiliate Member of UMSOM’s Institute for Genome Sciences. “Our extended analysis gives us very specific avenues to follow up on in future studies, as well as provides an encyclopedia that other researchers can use as a resource to study hearing loss.”
“As an otolaryngologist surgeon-scientist, I see patients with hearing loss due to age or noise damage, and I want to be able to help prevent or even reverse the damage to their hearing,” said study leader Ronna Hertzano, MD, PhD, Professor of Otorhinolaryngology-Head & Neck Surgery, Anatomy and Neurobiology at UMSOM and Affiliate Member of UMSOM’s Institute for Genome Sciences. “Our extended analysis gives us very specific avenues to follow up on in future studies, as well as provides an encyclopedia that other researchers can use as a resource to study hearing loss.”
The team added their newest data on noise-induced hearing loss to gEAR — Gene Expression Analysis Resource — a tool developed by her laboratory that allows researchers not trained in informatics to browse gene expression data (published earlier this summer).
Dr. Hertzano explained that the inner ear resembles the shell of a snail, with separate fluid compartments and sensory cells along its entire length. The ear functions like a battery with a gradient of ions between the fluid compartments that is generated by the side wall of the shell by adding in potassium. The sensory cells detect sound and then communicate with the neurons that interact with the brain to interpret the signal. The sensory cells are surrounded by support cells. The inner ear also has resident immune cells to protect it from infection.
Research Supervisor Beatrice Milon, PhD, in Dr. Hertzano’s laboratory initially did an analysis on the sensory cells and the support cells of the ear in mice. She collected data on the changes in gene expression from before and after noise damage. After making their study known to other researchers in their field, the team heard from scientists at Decibel Therapeutics (led by Joe Burns, PhD) and the Karolinska Institute (led by Barbara Canlon, PhD), who had the gene expression data from the inner ear’s neurons, side wall and immune cells from before and after noise damage. The teams then combined the datasets and performed their analysis.
The bioinformatic analyses were led by Eldad Shulman, MA, MS, from the lab of Ran Elkon, PhD, Tel Aviv University, a bioinformatics expert that has been working collaboratively with Dr. Hertzano now for over two decades. Together, they leverage advanced computational techniques and combine them with biological insights to analyze and interpret data, providing impactful insights to the hearing research field.
Dr. Hertzano says it was so important that they looked at a cell specific level, rather than looking at the entire ear because they found that most of the gene expression changes were specific to only one or two cell types.
“We expected the subset of neurons typically sensitive to noise and aging, to have “bad” changes in genes, so that we could counter them with drugs, but there was no such thing,” said Dr. Hertzano. “On the contrary, we found that the subset of neurons that are resistant to noise trauma, turn on a program that protects them while the very sensitive neurons had little change in gene expression. We are currently looking into approaches to induce the protective changes in the noise-sensitive neurons to prevent their loss from noise and aging.”
In another example, the researchers found that only one out of the four types of immune cells detected showed major differences in gene expression.
Additionally, immune-related genes were turned up in all cell types of the inner ear after noise damage with many of them controlled by two key regulators.
The research team took the overall gene expression trends and plugged them into DrugCentral, a database of known molecular responses to FDA-approved drugs, specifically searching for changes that would be opposite of those happening in the noise-damaged cells. They identified the diabetes drug metformin as a potential candidate, as well as some inhaled anesthetic medications used in surgeries and other medications.
 “Hearing aids and cochlear implants are used to alleviate hearing loss, however, there are no therapies available to prevent or treat hearing loss,” said E. Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor, and Dean, UMSOM. “The studies that follow up on these findings may eventually lead to medications to prevent occupational noise-induced hearing loss, for example in factory workers, and to changes in standardizing anesthesia protocols for ear surgery, particularly in hearing preservation procedures.”
“Hearing aids and cochlear implants are used to alleviate hearing loss, however, there are no therapies available to prevent or treat hearing loss,” said E. Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor, and Dean, UMSOM. “The studies that follow up on these findings may eventually lead to medications to prevent occupational noise-induced hearing loss, for example in factory workers, and to changes in standardizing anesthesia protocols for ear surgery, particularly in hearing preservation procedures.”
This work was funded by the National Institute on Deafness and Other Communication Disorders (R01DC013817, R01DC03544), the Department of Defense Congressionally Directed Medical Research Program (MR130240, RH200052), the Carolyn Frenkil Foundation, the Hearing Restoration Project of the Hearing Health Foundation, the Swedish Medical Research Council and Hörselforskningsfonden, the Karolinska Institutet, Tysta Skolan and Office of the Assistant Secretary of Defense for Health Affairs through the Neurosensory and Rehabilitation (W81XWH-16-1-0032), the European Union’s Horizon 2020 research and innovation programme (722046, 848261), the United States - Israel Binational Science Foundation (2017218), the Edmond J. Safra Center for Bioinformatics at Tel Aviv University, Teva Pharmaceutical Industries Ltd, and the Israeli National Forum for BioInnovators.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories

Friday, July 16, 2021
New High-Tech Portal Launched to Speed Innovations to Reverse Hearing Loss
Researchers at the University of Maryland School of Medicine (UMSOM) have launched a new online tool that could more quickly advance medical discoveries to reverse progressive hearing loss. The tool enables easy access to genetic and other molecular data from hundreds of technical research studies involving hearing function and the ear. The research portal called gene Expression Analysis Resource (gEAR, umgear.org) was unveiled in a study last month in Nature Methods. It is operated by a group of physician-scientists at the UMSOM Institute for Genome Sciences (IGS) in collaboration with their colleagues at other institutions.

Wednesday, November 21, 2018
UMSOM Expert Discovers Key Gene in Cells Associated with Age-Related Hearing Loss
An international group of researchers, led by Ronna Hertzano, MD, PhD, Associate Professor, Department of Otorhinolaryngology-Head & Neck Surgery, Anatomy and Neurobiology, at the University of Maryland School of Medicine (UMSOM), and Michael Bowl, Ph.D., Programme Leader Track Scientist, Mammalian Genetics Unit, MRC Harwell Institute, UK, have identified the gene that acts as a key regulator for special cells needed in hearing.

