September 30, 2020 | Deborah Kotz

Finding Could Lead to Future Treatments for Hearing Loss
Researchers at the University of Maryland School of Medicine (UMSOM) have conducted a study that has determined the role that a critical protein plays in the development of hair cells. These hair cells are vital for hearing. Some of these cells amplify sounds that come into the ear, and others transform sound waves into electrical signals that travel to the brain. Ronna Hertzano, MD, PhD, Associate Professor in the Department of Otorhinolaryngology Head and Neck Surgery at UMSOM and Maggie Matern, PhD, a postdoctoral fellow at Stanford University, demonstrated that the protein, called GFI1, may be critical for determining whether an embryonic hair cell matures into a functional adult hair cell or becomes a different cell that functions more like a nerve cell or neuron.
The study was published in the journal Development, and was conducted by physician-scientists and researchers at the UMSOM Department of Otorhinolaryngology Head and Neck Surgery and the UMSOM Institute for Genome Sciences (IGS), in collaboration with researchers at the Sackler School of Medicine at Tel Aviv University in Israel.
Hearing relies on the proper functioning of specialized cells within the inner ear called hair cells. When the hair cells do not develop properly or are damaged by environmental stresses like loud noise, it results in a loss of hearing function.
In the United States, the prevalence of hearing loss doubles with every 10-year increase in age, affecting about half of all adults in their 70s and about 80 percent of those who are over age 85. Researchers have been focusing on describing the developmental steps that lead to a functional hair cell, in order to potentially generate new hair cells when old ones are damaged.
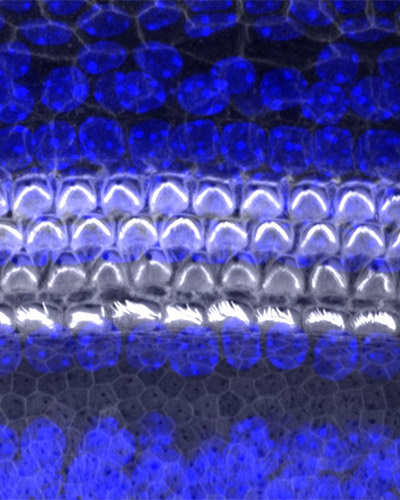 To conduct her latest study, Dr. Hertzano and her team utilized cutting-edge methods to study gene expression in the hair cells of genetically modified newborn mice that did not produce GFI1. They demonstrated that, in the absence of this vital protein, embryonic hair cells failed to progress in their development to become fully functional adult cells. In fact, the genes expressed by these cells indicated that they were likely to develop into neuron-like cells.
To conduct her latest study, Dr. Hertzano and her team utilized cutting-edge methods to study gene expression in the hair cells of genetically modified newborn mice that did not produce GFI1. They demonstrated that, in the absence of this vital protein, embryonic hair cells failed to progress in their development to become fully functional adult cells. In fact, the genes expressed by these cells indicated that they were likely to develop into neuron-like cells.
“Our findings explain why GFI1 is critical to enable embryonic cells to progress into functioning adult hair cells,” said Dr. Hertzano. “These data also explain the importance of GFI1 in experimental protocols to regenerate hair cells from stem cells. These regenerative methods have the potential of being used for patients who have experienced hearing loss due to age or environmental factors like exposure to loud noise.”
Dr. Hertzano first became interested in GFI1 while completing her M.D., Ph.D. at Tel Aviv University. As part of her dissertation, she discovered that the hearing loss resulting from mutations in another protein called POU4F3 appeared to largely result from a loss of GFI1 in the hair cells. Since then, she has been conducting studies to discover the role of GFI1 and other proteins in hearing. Other research groups in the field are now testing these proteins to determine whether they can be used as a “cocktail” to regenerate lost hair cells and restore hearing.
“Hearing research has been going through a Renaissance period, not only from advances in genomics and methodology, but also thanks to its uniquely collaborative nature among researchers,” said Dr. Herzano.
The new study was funded by the National Institute on Deafness and Other Communication Disorders (NIDCD) which is part of the National Institutes of Health (NIH). It was also funded by the Binational Scientific Foundation (BSF).
“This is an exciting new finding that underscores the importance of basic research to lay the foundation for future clinical innovations,” said E. Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor and Dean, University of Maryland School of Medicine. "Identifying the complex pathways that lead to normal hearing could prove to be the key for reversing hearing loss in millions of Americans.”
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 45 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has more than $540 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 student trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of nearly $6 billion and an economic impact more than $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th highest among public medical schools in research productivity, is an innovator in translational medicine, with 600 active patents and 24 start-up companies. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Deborah Kotz
410-706-4255
dkotz@som.umaryland.edu
Related stories

Wednesday, February 22, 2023
University of Maryland School of Medicine Professor Appointed Chief of New Branch at NIH
Ronna Hertzano, MD, PhD, Professor of Otorhinolaryngology-Head & Neck Surgery, at the University of Maryland School of Medicine (UMSOM) has been appointed as Chief of the newly established Neurotology Branch in The National Institute on Deafness and Other Communication Disorders (NIDCD).

Friday, April 09, 2021
Lowering Music Volume at Group Spin Classes Does Not Affect Intensity of Workouts, UM School of Medicine Researchers Find
Fitness center instructors often turn up music volumes significantly during classes sometimes loud enough to cause hearing damage -- based on an assumption that participants will work out more intensively when volumes are raised. A new University of Maryland School of Medicine (UMSOM) study, however, found that those who attend indoor cycling (“spinning”) classes do not lower the intensity of their workouts when the volume is reduced to a safer decibel level. The findings were published today in the journal Noise & Health.

Thursday, August 03, 2017
UM SOM Study Announces Breakthrough in Understanding Hearing Loss
Researchers at the University of Maryland School of Medicine (UM SOM) today announced a breakthrough discovery that could eventually help scientists repair hearing problems or protect those at risk for hearing loss – a condition that affects some 40 million Americans.
