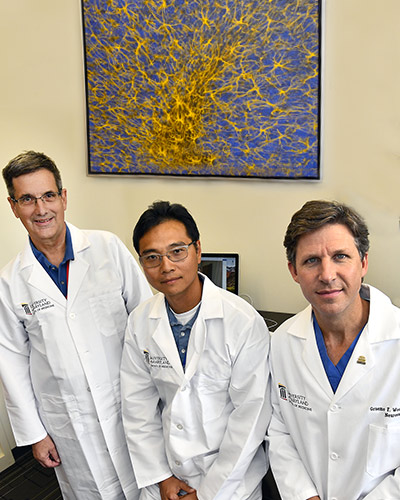
January 15, 2020 | Deborah Kotz
Experimental Nanoformulation Outperforms FDA-Approved Treatment for Metastatic Breast Cancer, Increasing Survival in Animal Studies
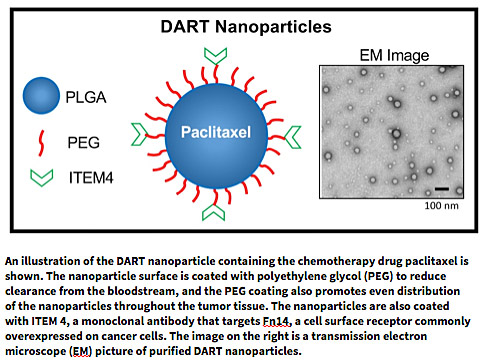
Researchers at the University of Maryland School of Medicine (UMSOM) developed a new nanoparticle drug formulation that targets a specific receptor on cancer cells and appears to be more effective than a standard nanoparticle therapy currently on the market to treat metastatic breast cancer, according to a study published today in the journal Science Advances. The new ‘DART’ nanoparticles bypass healthy cells and tissues and bind to tumor cells, dispersing evenly throughout the tumor while releasing the chemotherapy drug paclitaxel.
“The marketed drug Abraxane, a nanoformulation containing paclitaxel that is currently used to treat women with aggressive breast cancer, is an effective agent, but it was not designed to selectively deliver paclitaxel to only the cancerous cells within the body,” said study corresponding co-author Jeffrey Winkles, PhD, a Professor of Surgery at UMSOM. “Our DART nanoparticle specifically targets the Fn14 receptor found abundantly on breast cancer cells; it uses this receptor to gain entry through the plasma membrane and deliver the drug to destroy the cancer.” Dr. Winkles’ group discovered the Fn14 receptor and described its potential as a target for new therapeutics more than a decade ago.
For this study, UMSOM researchers engineered and tested a new therapeutic nanoparticle platform to deliver the drug paclitaxel to treat triple-negative breast cancer. About one in five women with breast cancer have this type of aggressive tumor, which is particularly difficult to treat; these cancers lack receptors commonly expressed by most breast cancer cells, like hormone receptors, for which effective drugs have been designed. But many triple-negative breast cancers express high levels of Fn14; indeed, most solid tumor types, including lung, prostate and colorectal cancer, overexpress this cell surface receptor.
 “After much initial hype and some disappointments in the field, nanoparticle delivery systems for cancer treatment are starting to show real promise for patients,” said study co-author Graeme Woodworth, MD, Professor and Interim Chair in the Department of Neurosurgery at UMSOM. “We established a proof-of-concept with this study, outlining the design of an optimized nanoparticle delivery system that balances the specific binding to cancer cells while minimizing non-specific, off-target binding to other cells in a very fine-tuned way.”
“After much initial hype and some disappointments in the field, nanoparticle delivery systems for cancer treatment are starting to show real promise for patients,” said study co-author Graeme Woodworth, MD, Professor and Interim Chair in the Department of Neurosurgery at UMSOM. “We established a proof-of-concept with this study, outlining the design of an optimized nanoparticle delivery system that balances the specific binding to cancer cells while minimizing non-specific, off-target binding to other cells in a very fine-tuned way.”
To accomplish this, the research team attached a monoclonal antibody called ITEM 4 to the surface of the nanoparticle because it specifically binds to Fn14, providing a key to unlock entry into the cancer cell. The surface of the nanoparticles was also coated with polyethylene glycol to keep them circulating through the bloodstream and lymph system until they reached the tumor and to prevent them from being quickly flushed out of the body.
“Many drug delivery carriers exhibit nonspecific binding to healthy cells and tissues in addition to the diseased cells they are targeting, which often leads to unintended side effects or toxicities,” said study corresponding co-author Anthony Kim, PhD, Associate Professor of Neurosurgery and Pharmacology at UMSOM. “This DART nanoparticle platform has unique capabilities to improve therapeutic delivery to difficult-to-treat locations within the body, while also allowing us to potentially increase the maximum tolerated dose of the encapsulated drug without increasing side effects to patients.”
The researchers filled their optimized DART nanoparticle formulation with paclitaxel and tested it against Abraxane (the marketed nanoparticle which also contains paclitaxel) in animals with triple-negative breast cancer tumors. In one set of experiments, the nanoparticles were delivered to mice harboring breast tumors grown above the natural breast region. They found the DART formulation led to a significantly increased median overall survival (68 days) compared to Abraxane treatment (45 days). They also saw a clear benefit to using the DART nanoparticles when they compared the treatments again in animals that harbored breast tumors implanted in the brain (akin to a metastatic brain tumor).
 “This is a compelling finding and significant step forward in the use of nanoparticles to treat cancer,” said UMSOM Dean E. Albert Reece, MD, PhD, MBA, University Executive Vice President for Medical Affairs and the John Z. and Akiko K. Bowers Distinguished Professor. “It fits squarely with our School of Medicine’s mission to advance the field of potentially lifesaving therapies for patients with the most difficult to treat cancers.”
“This is a compelling finding and significant step forward in the use of nanoparticles to treat cancer,” said UMSOM Dean E. Albert Reece, MD, PhD, MBA, University Executive Vice President for Medical Affairs and the John Z. and Akiko K. Bowers Distinguished Professor. “It fits squarely with our School of Medicine’s mission to advance the field of potentially lifesaving therapies for patients with the most difficult to treat cancers.”
The UMSOM researchers are members of the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center. A former Ph.D. student, Jimena Dancy, PhD, and a former Postdoctoral Fellow, Aniket Wadajkar, PhD, are listed as co-first authors on the publication. Researchers from the Translational Genomics Research Institute in Phoenix, Arizona and the Mayo Clinic Arizona in Scottsdale also contributed to the work.
This study was primarily funded by the National Institutes of Health.
Future research includes testing the DART therapy in other cancer types, including an aggressive form of brain cancer called glioblastoma and developing a similar version of the nanoparticle designed to work specifically in humans. This would involve using a humanized antibody on the surface of the nanoparticle and scaling up the formulation. The researchers recently received a grant from the TEDCO Maryland Innovation Initiative Commercialization Program to move forward with efforts to adapt their nanoparticle system and eventually test the treatment in cancer patients.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 45 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has more than $540 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 student trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of nearly $6 billion and an economic impact more than $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th highest among public medical schools in research productivity, is an innovator in translational medicine, with 600 active patents and 24 start-up companies. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Deborah Kotz
Director of Media Relations
Office of Public Affairs & Communications
University of Maryland School of Medicine
o: 410-706-4255
c: 410-804-0054
t: @debkotz2
Related stories

Monday, August 25, 2025
University of Maryland School of Medicine Researchers Detail Reliable Measurement for Blood-Brain Barrier Opening Using Focused Ultrasound
Researchers from the University of Maryland School of Medicine (UMSOM), Brigham and Women’s Hospital in Boston and other North American institutions, have provided the first technical description for using focused ultrasound to reliably open the blood-brain barrier. The findings, recently published in Device, pave the way for expanding the use of this experimental device to open the blood-brain barrier to improve treatments and diagnostics for patients with brain tumors and other neurological disorders.

Monday, December 12, 2022
University of Maryland School of Medicine Launches New Maryland Institute for Neuroscience Discovery (UM-MIND)
University of Maryland School of Medicine (UMSOM) Dean Mark T. Gladwin, MD, has announced plans to launch a new neuroscience institute that will accelerate translational research of the brain by facilitating interaction between basic and clinical scientists and enhancing collaborative research across the UMSOM and University of Maryland, Baltimore (UMB) campus.
Thursday, August 09, 2018
University of Maryland School of Medicine Scientists to Conduct First FDA-Approved Study of Focused Ultrasound to Open Blood-Brain Barrier
In the first such clinical trial in the United States, physician-scientists with the University of Maryland School of Medicine (UMSOM) are investigating the use of MRI-guided focused ultrasound to open the blood-brain barrier. The trial will be conducted with patients undergoing brain cancer surgery at the University of Maryland Medical Center (UMMC).
