March 27, 2019 | Joanne Morrison

Dr. Todd Gould’s Research Helps Uncover How Certain Receptors Play Role in the Mechanism of Fast-Acting Antidepressants
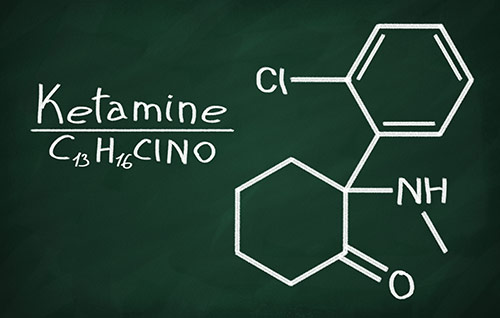
Effective treatment of clinical depression remains a major mental health issue, with roughly 30 percent of patients who do not respond to any of the available treatments. Researchers at the University of Maryland School of Medicine (UMSOM) have discovered a crucial receptor called mGlu2 that is critical to the mechanism of fast-acting antidepressants such as ketamine when used to treat depression.
This discovery into how this type of receptor in the brain works with fast-acting antidepressants is a critical discovery in treating depression, because existing treatments can take weeks before they are effective. A single dose of ketamine that is lower than the amount required to cause anesthesia within 24 hours can alleviates depression in some treatment-resistant patients.
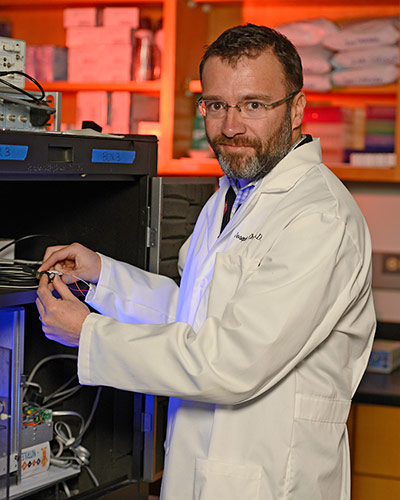
Todd Gould, MD., Associate Professor in the Department of Psychiatry, together with researchers from the National Institutes of Health Intramural Research Program, discovered that this special type of glutamate receptor interacts with ketamine’s mechanism.
“Understanding the neurological response to antidepressants such as ketamine help us better understand depression and how to best treat this serious disease,” said Dr. Gould.
The effects of ketamine can last up to a few weeks. And while it is a fast-acting treatment for depression, it is not an ideal treatment because it can alter sensory perception and has a high potential for abuse. Thus, there is a tremendous need to identify the mechanisms through which ketamine mediates its antidepressant effects to help identify alternative drugs that more specifically enhance the pathway in the brain that is suppressed in depressed patients.
 Necessary Receptors
Necessary Receptors
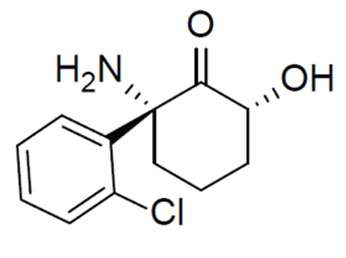
Dr. Gould’s research, which was conducted in mice, showed that the mGlu2 receptor is necessary of the antidepressant activity of ketamine, and the ketamine metabolite. Researchers were able to uncover the important role this receptor plays in ketamine effectiveness by removing the gene for this receptor in mice, which in turn blocked the antidepressant effects of fast-acting treatment. Additionally, Dr. Gould’s research provided evidence that an increase in a particular form of brain activity, measured by quantitative EEG, can be used as an indicator of on-target activity of fast-acting antidepressants.
The researchers used mice to determine that (2R, 6R)-HNK’s mechanism of action involved mGlu2 receptors. Various experimental strategies were applied, including pharmacological manipulation of mGlu2 activity, genetic knockout of the mGlu2-encoding gene, behavioral tests, and cortical EEG measurements.
“Having a better understanding of how the brain reacts to Ketamine is a critical pathway toward advancing treatment of Depression,” said UMSOM Dean E. Albert Reece, MD, PhD, MBA, who is also the Executive Vice President for Medical Affairs, University of Maryland, and the John Z. and Akiko K. Bowers Distinguished Professor.
The research was funded by the National Institutes of Health, a Veterans Affairs Merit Award, a Harrington Discovery Institute Scholar-Innovator grant and the Kahlert Foundation.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 43 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished recipient of the Albert E. Laser Award in Medical Research. With an operating budget of more than $1 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically-based care for more than 1.2 million patients each year. The School has over 2,500 students, residents, and fellows, and more than $530 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total workforce of nearly 7,000 individuals. The combined School and Medical System (“University of Maryland Medicine”) has an annual budget of nearly $6 billion and an economic impact more than $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th highest among public medical schools in research productivity, is an innovator in translational medicine, with 600 active patents and 24 start-up companies. The School works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu/
Contact
Department of Anesthesiology
(410) 328-6120 (phone)
(410) 328-5531 (fax)
swalsh@som.umaryland.edu
Joanne Morrison
Director of Marketing and Public Relations
University of Maryland School of Medicine
jmorrison@som.umaryland.edu
Office: (410) 706-2884
Mobile: (202) 841-3369
Related stories

Tuesday, August 30, 2022
Effects of Drugs in Mice can Depend on the Sex of the Human Experimenter
University of Maryland School of Medicine researchers demonstrated that a stress response in the brain is essential for ketamine’s antidepressant response in mice suggesting new ways to improve antidepressant therapy for patients who do not respond to the treatment.

Tuesday, May 10, 2022
Longtime Academic and Clinical Affairs Leader, Department Chair, and Faculty Member, Tony Lehman, MD, Announces Retirement
University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, announced today that Anthony Lehman, MD, MSPH, who served the UMSOM for more than 30 years as Senior Associate Dean for Clinical Affairs, Department Chair, and distinguished faculty member in the UMSOM Department of Psychiatry, will retire, effective June 30, 2022.
Tuesday, April 13, 2021
UM School of Medicine Study Shows that Psychedelic Experience May Not be Required for Psilocybin’s Antidepressant-like Benefits
University of Maryland School of Medicine (UMSOM) researchers have shown that psilocybin—the active chemical in “magic mushrooms”— still works its antidepressant-like actions, at least in mice, even when the psychedelic experience is blocked. The new findings suggest that psychedelic drugs work in multiple ways in the brain, and it may be possible to deliver the fast-acting antidepressant therapeutic benefit without requiring daylong guided-therapy sessions.

Thursday, February 27, 2020
UMSOM Department of Psychiatry Creates New Position to Strengthen and Support Research Program
Jill RachBeisel, MD, Interim Chair of the Department of Psychiatry at the University of Maryland School of Medicine (UMSOM), along with UMSOM Dean E. Albert Reece, MD, PhD, MBA, announced today that Gloria Reeves, MD, Associate Professor of Psychiatry, has been appointed to serve as the Vice Chair for Research of the Department.

Thursday, January 16, 2020
University of Maryland School of Medicine Research Shows That Older Patients With Untreated Sleep Apnea Need Greater Medical Care
Obstructive sleep apnea (OSA) is a common and costly medical condition leading to a wide range of health risks such as cardiovascular disease, stroke, depression, diabetes and even premature death. Researchers at the University of Maryland School of Medicine (UMSOM) found that the medical costs are substantially higher among older adults who go untreated for the disorder.
Wednesday, October 16, 2019
Researchers Discover Potential Therapy to Treat Detrimental Effects of Marijuana in Pre-Adolescent Individuals Exposed to THC in Womb
As a growing number of U.S. states legalize the medicinal and recreational use of marijuana, an increasing number of American women are using cannabis before becoming pregnant and during early pregnancy often to treat morning sickness, anxiety, and lower back pain. Although emerging evidence indicates that this may have long-term consequences for their babies’ brain development, how this occurs remains unclear.

Thursday, April 04, 2019
Mobile Addiction Treatment Unit Serves Maryland Eastern Shore
Health and addiction treatment officials from the Caroline County Health Department, Maryland Department of Health, the Maryland Opioid Operational Command Center, and the University of Maryland School of Medicine (UMSOM) in Denton, MD., launched the Eastern Shore Mobile Care Collaborative (ESMCC), a mobile system designed to provide state-of-the-art treatment for opioid disorders for those in need on the Maryland Eastern shore.
Tuesday, October 16, 2018
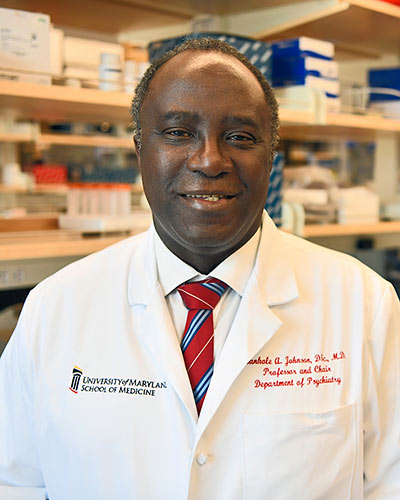
Bankole A. Johnson Receives Prestigious American Society of Addiction Medicine Award
Bankole Johnson, DSc, MD, the Dr. Irving J. Taylor Professor and Chair of the Department of Psychiatry at the University of Maryland School of Medicine (UMSOM), has been named to receive the American Society of Addiction Medicine’s (ASAM) R. Brinkley Smithers Distinguished Scientist Award.

Friday, January 05, 2018
Fighting Opioid Addiction from Baltimore to Garrett County: University of Maryland School of Medicine Rises to the Challenge
The opioid epidemic has been deadly for Maryland. In 2016, more than 2000 people in the state died from overdoses; in 2017, deaths rose another 40 percent, and deaths from the powerful synthetic opioid fentanyl were up nearly 140 percent. Last year, Gov. Larry Hogan declared a state of emergency in response to the opioid epidemic, saying the state needs an “all-hands-on-deck approach.”
Wednesday, June 07, 2017
Dr. Jill RachBeisel Named Vice Chair for Clinical Affairs in UM School of Medicine’s Department of Psychiatry
Bankole A. Johnson, DSc, MD, MBChB, The Dr. Irving J. Taylor Professor and Chair for the Department of Psychiatry, Professor of Pharmacology, Anatomy and Neurobiology, along with UM SOM Dean E. Albert Reece, MD, PhD, MBA, announced today that Jill RachBeisel, MD, Associate Professor of Psychiatry, has been named Vice Chair for Clinical Affairs for the UM SOM Department of Psychiatry, commencing at the start of the next academic year.
Wednesday, May 04, 2016
UM SOM Researchers Identify Potentially Revolutionary Antidepressant Compound
For years, scientists and doctors have known that ketamine can treat depression very rapidly, often working within hours, compared to weeks or months for widely used antidepressants. However, the drug, which is approved as an anesthetic, has major side effects – it is linked to hallucinations and dissociation - a sense of being outside your own body – and for these reasons is abused as a club drug. Not surprisingly, this limits its use in the treatment of depression.
