March 27, 2019

University of Maryland School of Medicine Research Could Set Path for Preventing Premature Births
Spontaneous preterm birth (sPTB), defined as birth before 37 weeks of gestation, and the related complications, are the largest contributors to infant death in the United States and worldwide, according to the World Health Organization. Researchers at the University of Maryland School of Medicine (UMSOM) have discovered that bacteria and innate immune factors in a woman’s birth canal and cervix may increase the risk of spontaneous preterm birth or provide protection against such births.
Results of the study, which was conducted in collaboration with the Perelman School of Medicine at the University of Pennsylvania, were published today in Nature Communications. This groundbreaking research provides information that could help physicians better predict and prevent these preterm births. The study sets the path for new research to develop rational strategy that would target “bad” bacteria or increase “protective” bacteria.
The findings are key as babies who survive an early birth often face serious, costly and lifelong health problems, including breathing problems, vision loss, cerebral palsy and intellectual delays. The economic burden of preterm birth is staggering, with an estimated cost of $26 billion per year in the United States alone, according to the National Academy of Sciences estimates. A failure to predict and understand the causes of preterm birth have limited the development of effective interventions and therapeutics.
In this study, researchers examined vaginal swabs from a sample of 2,000 pregnant women taken at three distinct points in pregnancy to determine the bacteria that made up the cervicovaginal microbiota. This is the largest cohort of pregnant women in whom the cervicovaginal microbiota was studied. Using innovative modeling of the cervicovaginal microbiota, seven bacteria were significantly associated with increased risk of spontaneous preterm birth, with a stronger effect seen in African American women. Interestingly, higher vaginal levels of the antimicrobial peptide β-defensin-2, a part of our innate immune system, lowered the risk of sPTB associated with cervicovaginal microbiota in an ethnicity-dependent manner.
"Predicting prematurity has been a riddle that has troubled researchers and clinicians for years, but we are finally shedding light on a path toward offering treatment to women we can identify as being at risk. Previous studies, including ours, were limited by low sample size. In establishing this large cohort, we aim to identify factors early in pregnancy that could be used to predict the risk to spontaneous preterm birth," said co-senior author Jacques Ravel, PhD, Professor of Microbiology and Immunology and Senior Scientist at the Institute for Genome Sciences (IGS), Director of Genomics, at the University of Maryland School of Medicine. “These new findings are the result of a multidisciplinary team of experts in obstetrics and microbiology, who came together and took a new approach to address this major problem in the United States and the world”
These findings hold promise for diagnostics to accurately identify women at risk for sPTB early in pregnancy. Therapeutic strategies could include immune modulators and microbiome-based therapeutics to reduce this significant health burden.
"Approaching this complex health problem of preterm births from a multidisciplinary perspective is given clinicians new insights," said UMSOM Dean E. Albert Reese, MD, PhD, MBA, who is also the Executive Vice President for Medical Affairs, University of Maryland and the John Z. and Akiko K. Bowers Distinguished Professor. "While there is known racial disparity in preterm births with African-American women having significantly higher rates than non-African American women, factors that underpin this disparity have remained elusive."
Dr. Ravel collaborated with Michal Elovitz, MD, professor, Obstetrics & Gynecology at the Perelman School at the University of Pennsylvania.
This study was supported by the National Institute for Nursing Research of the National Institutes of Health under award number R01NR014784.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 43 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished recipient of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for more than 1.2 million patients each year. The School has over 2,500 students, residents, and fellows, and more than $530 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total workforce of nearly 7,000 individuals. The combined School and Medical System (“University of Maryland Medicine”) has an annual budget of nearly $6 billion and an economic impact more than $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th highest among public medical schools in research productivity, is an innovator in translational medicine, with 600 active patents and 24 start-up companies. Th School works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu.
About the Institute for Genome Sciences
The Institute for Genome Sciences, founded in 2007, is an international research center within the University of Maryland School of Medicine. Comprised of an interdisciplinary, multidepartment team of investigators, the Institute uses the powerful tools of genomics and bioinformatics to understand genome function in health and disease, to study molecular and cellular networks in a variety of model systems, and to generate data and bioinformatics resources of value to the international scientific community.
igs.umaryland.edu
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Related stories

Wednesday, August 28, 2024
Leading Computational Scientist and Oncology Researcher Elana Fertig, PhD, Appointed as New Director of the Institute for Genome Sciences at the University of Maryland School of Medicine
University of Maryland School of Medicine (UMSOM) Dean Mark T. Gladwin, MD, announced today the appointment of Elana J. Fertig, PhD, FAIMBE, as the new Director of the School’s Institute for Genome Sciences (IGS). She is an internationally-recognized researcher known for her work in integrating spatial multi-omics technologies with mathematical models to develop a new predictive medicine paradigm in cancer. Spatial technologies allow researchers to learn about any cell type inside of natural tissue, including gene activity and cell interactions.

Thursday, July 28, 2022
Researchers Discover One of the Largest Known Bacteria-to-Animal Gene Transfer Inside a Fruit Fly
A fruit fly genome is not a just made up of fruit fly DNA – at least for one fruit fly species. New research from the University of Maryland School of Medicine’s (UMSOM) Institute for Genome Sciences (IGS) shows that one fruit fly species contains whole genomes of a kind of bacteria, making this finding the largest bacteria-to-animal transfer of genetic material ever discovered. The new research also sheds light on how this happens.

Monday, September 20, 2021
UM School of Medicine Receives $7.5 Million Grant to Create Complex Model of Female Reproductive Tract to Study Infections
Researchers at the Institute for Genome Sciences (IGS) at the University of Maryland School of Medicine have received a $7.5 million federal grant to create a complex model of the female reproductive system in order to study sexually transmitted infections (STIs). They plan to create a realistic 3D model that integrates vaginal and cervical epithelial cells and the bacteria that colonize these cells, called a microbiome. They aim to use this model to identity factors that play a role in chlamydia and gonorrhea infections experienced by a growing number of women in the U.S. and worldwide.

Thursday, March 18, 2021
UM School of Medicine Helps Maryland Conduct State-Wide Sequencing of Variants in Positive COVID-19 Test Specimens
In an effort to monitor the spread of COVID-19 variants in the State of Maryland, University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, announced that UMaryland Genomics at UMSOM will perform genome sequencing of variants in at least 10 percent of COVID-19 test samples, reaching an important benchmark set by the federal government to help control the spread of these variants.

Tuesday, December 03, 2019
UM School of Medicine Researchers Institute for Genome Sciences' Researchers Discover Potential New Treatment for Tropical Parasitic Disease Using Genomics
Using innovative RNA sequencing techniques, researchers at the University of Maryland School of Medicine (UMSOM) Institute for Genome Sciences identified a promising novel treatment for lymphatic filariasis, a disabling parasitic disease that is difficult to treat. The potential new therapy is an experimental cancer drug called JQ1 and targets proteins found prominently in the worm’s genome; it appears to effectively kill the adult worms in a laboratory setting, according to the study which was published today in the journal mSystems.

Tuesday, August 13, 2019
Researchers Identify How Vaginal Microbiome Can Elicit Resistance or Susceptibility to Chlamydia
The vaginal microbiome is believed to protect women against Chlamydia trachomatis, the etiological agent of the most prevalent sexually transmitted infections (STIs) in developed countries. New research by the University of Maryland School of Medicine (UMSOM) shows how the microbiome can either protect or make a woman more susceptible to these serious infections.

Thursday, April 04, 2019
UM School of Medicine's Institute for Genome Sciences Awarded $17.5 Million Grant for Infectious Disease Research
The Institute for Genome Sciences (IGS) at the University of Maryland School of Medicine (UMSOM) was awarded $17.5 million from the National Institute of Allergy and Infectious Diseases (NIAID) to fund the IGS Genome Center for Infectious Diseases (GCID) for another five years.

Tuesday, February 12, 2019
UMSOM Scientists Call for Unrestricted Usage of Public Genome Data
Researchers at the Institute for Genome Sciences (IGS) at the University of Maryland School of Medicine (UMSOM) called for open access to genome data, stating that unrestricted usage is needed for progress in combating the world’s most serious diseases.
Friday, February 08, 2019
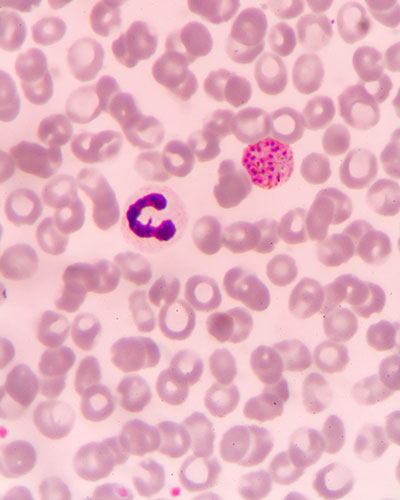
University of Maryland School of Medicine Genome Scientists Develop Novel Approaches to Studying the Most Widespread Form of Malaria
Scientists at the Institute of Genome Sciences (IGS) at the University of Maryland School of Medicine (UMSOM) have developed a novel way with genome sequences to study and better understand transmission, treat and ultimately eradicate Plasmodium vivax, the most widespread form of malaria.

Thursday, September 27, 2018
University of Maryland School of Medicine Scientist Receives Prestigious Microbiome Award
Owen White, PhD, professor of epidemiology and public health, and Associate Director for Informatics at the Institute for Genome Sciences (IGS) at the University of Maryland School of Medicine (UMSOM), has received the 2018 Microbiome Pioneer Award. The prestigious honor is part of the Bioinformatics for the Microbiome Symposium organized by Stanford University. The microbiome is the name given collectively to the community of trillions of microbial organisms that live on and within our bodies.
Monday, May 14, 2018
New Research: Some Gut Bacteria May Protect Against Intestinal Infection
Scientists at the University of Maryland School of Medicine (UMSOM) have for the first time found evidence that the presence of a key species in the human gut microbiome is associated with protection from infection with typhoid fever. If the research is borne out, it could offer an exciting new way to reduce intestinal infections from microbes.
Wednesday, May 25, 2016
UMSOM Researchers Develop New Way to Decode Large Amounts of Biological Data
A University of Maryland School of Medicine researcher has helped develop an innovative computing technique that, on very large amounts of data, is both faster and more accurate than current methods. To spur research, a program using this technique is being offered for free to the biomedical research community.
