September 28, 2017

Study Uncovers a Previously Unknown Molecular Bridge Between Sleep and Memory
More than 3.2 million Americans suffer from schizophrenia; about 100,000 people are newly diagnosed every year. The disease includes a wide range of symptoms including visual and auditory hallucinations, cognitive problems and motivational issues. A key issue with the disease, and one that gets less attention than other symptoms, is cognitive problems. Many with the disease have trouble with learning and memory. For many, this is the first sign of the disease.
A new study by researchers at the (UM SOM) has found intriguing links between sleep, cognition and a compound called kynurenine. These links could illuminate the mechanism that causes cognitive problems among those with the disease, and could point the way to new treatments to reduce some of the disease’s symptoms.
The findings were published today in the journal Sleep. The study is the first to illuminate in detail the links between kynurenine, its metabolite kynurenic acid, sleep and cognition.
“No one has looked closely at the relationship between sleep and the kynurenine pathway before,” said Ana Pocivavsek, PhD, a researcher at the UM SOM Maryland Psychiatric Research Center (MPRC) and an assistant professor in the Department of Psychiatry. “This research establishes a clear link between elevations in kynurenine and sleep problems.”
In recent years, scientists have identified kynurenic acid as a potential key player in schizophrenia. Kynurenic acid is a neuroactive metabolite of kynurenine that is formed in the brain. People with schizophrenia have higher than normal levels of kynurenic acid in their brains. Scientists have theorized that these elevated levels might be connected with a range of symptoms seen in the disease, including problems with learning and memory.
The mechanisms underlying the cognitive impairments in patients, however, have remained unclear. Dr. Pocivavsek and her colleagues suspected that an interplay between elevated kynurenic acid and sleep could play a role. There is a lot of evidence in both humans and animals that sleep dysfunction leads to problems with learning and memory. In addition, researchers and clinicians have long noted that people with schizophrenia often have problems with sleep as well.
For these experiments, she and her colleagues studied rats. They made comparisons in the behavior of rats with increased kynurenic acid in their brains to animals with normal levels of the compound. They connected the animals’ brains to a device that measured the amount and quality of sleep, and found that the animals with higher levels of kynurenic acid had significantly less rapid eye movement, or REM, sleep. This is the sleep phase in which dreams occur, and it is thought to be critical for the consolidation of previous learning.
The researchers found that the group with high kynurenic acid also had problems with learning. To test this, they place rats in a box and shine light into the box. On one side of the box there is an opening into a darker area. Rats are nocturnal animals, and prefer the dark, so the animals typically run to the dark area. Once in this area, they receive a small electric shock. When the experiment is repeated the next day, normal animals do not run to the darker area, remembering the shock from the day before. By comparison, animals with increased levels of high kynurenic acid, and thus impaired sleep, do not remember the shock from the day before, and run into the dark area. In other words they did not learn from the previous day’s experience.
“What we’re starting to think about is that kynurenic acid disrupts sleep, which then disrupts cognition,” she said. However, there are other possibilities, she says: it may be that disruptions in sleep cause increased kynurenic acid, which then leads to cognitive problems. “It’s not clear which happens first,” she says. “That is a really interesting question, and one that we are investigating.”
Dr. Pocivavsek and other researchers theorize that reducing kynurenic acid could reduce problems with sleep and cognition in patients with schizophrenia. “We certainly believe that high levels of kynurenic acid are a crucial aspect of schizophrenia,” she says.
The research provides more reason to develop medicines that reduce kynurenic acid levels in the brain. One key possibility is to inhibit an enzyme called kynurenine aminotransferase II, or KAT II, which converts kynurenine to kynurenic acid. Using compounds that inhibit this enzyme, researchers have been able to reduce the amount of kynurenic acid in the brain. Over the years, various pharmaceutical companies have worked to develop inhibitors of KAT II that can reach the brain, and would be safe and effective in humans. Dr. Pocivavsek’s research provides evidence that this approach has clinical potential.
“This study adds to the evidence that high levels of kynurenic acid contribute to cognitive dysfunction,” she says. “If we can come up with ways to reduce those levels, we may be able to reduce these symptoms for patients.”
 Dr. Pocivavsek collaborated on the research with Jessica A. Mong, PhD, an associate professor in the Department of Pharmacology, who has previously done research on cellular and molecular mechanisms underlying sleep and arousal states. Research assistants Annalisa Baratta and Shaun Viechweg also contributed to the study.
Dr. Pocivavsek collaborated on the research with Jessica A. Mong, PhD, an associate professor in the Department of Pharmacology, who has previously done research on cellular and molecular mechanisms underlying sleep and arousal states. Research assistants Annalisa Baratta and Shaun Viechweg also contributed to the study.
“Schizophrenia not only affects patients, but their families as well. It is an extremely difficult disease, and this innovative work by Dr. Pocivavsek and her colleagues offers hope that in the future we can develop new approaches to some of the most pernicious symptoms,” said UM SOM Dean E. Albert Reece, MD, PhD, MBA, who is also the vice president for Medical Affairs, University of Maryland, and the John Z. and Akiko K. Bowers Distinguished Professor. “Once again we see the unbreakable link between basic research and helping patients.”
About the University of Maryland School of Medicine
Commemorating its 210th Anniversary, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 43 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academies of Science, Engineering and Medicine, and a distinguished recipient of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically-based care for more than 1.2 million patients each year. The School has over 2,500 students, residents, and fellows, and nearly $450 million in extramural funding, with more than half of its academic departments ranked in the top 20 among all public medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has nearly 7,000 total employees. The combined School and Medical System (“University of Maryland Medicine”) has a total budget of $5 billion and an economic impact of nearly $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th-highest public medical school in research productivity, is an innovator in translational medicine with 600 active patents and 24 start-up companies. The School works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu/
Learn More
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Related stories

Thursday, January 08, 2026
Improving Sleep Isn’t Enough: Researchers Highlight Daytime Function as Key to Assessing Insomnia Treatments
About one in nine adults suffer from chronic insomnia and its residual effects like drowsiness, cognitive issues, and irritability as well as increased health risks like diabetes and heart risks if left untreated. While many treatments are available, the challenge lies in determining how well a medication or other sleep aid works in individual patients.

Thursday, November 21, 2024
UM School of Medicine Researchers Link Snoring to Behavioral Problems in Adolescents without Declines in Cognition
Adolescents who snore frequently were more likely to exhibit behavior problems such as inattention, rule-breaking, and aggression, but they do not have any decline in their cognitive abilities, according to a new study conducted by researchers at the University of Maryland School of Medicine (UMSOM). This is the largest study to date tracking snoring in children from elementary school through their mid-teen years and it provides an important update to parents struggling with what medical measures to take to help manage snoring in their children.
Friday, July 29, 2022
Children Who Lack Sleep May Experience Detrimental Impact on Brain and Cognitive Development That Persists Over Time, UM School of Medicine Study Finds
Elementary school-age children who get less than nine hours of sleep per night have significant differences in certain brain regions responsible for memory, intelligence, and well-being compared to those who get the recommended 9-12 hours of sleep per night, according to a new study led by University of Maryland School of Medicine (UMSOM) researchers. Such differences correlated with greater mental health problems like depression, anxiety, and impulsive behaviors in those who lacked sleep. Inadequate sleep was also linked to cognitive difficulties with memory, problem solving and decision making. The findings were published today in the journal Lancet Child & Adolescent Health.

Tuesday, October 31, 2017
UM SOM Professor of Psychiatry Recognized for Innovative and Promising Research in Schizophrenia
Deanna Kelly, PharmD, BCPP, Professor of Psychiatry at the University of Maryland School of Medicine (UM SOM), has been awarded the 2017 Maltz Prize for Innovative and Promising Schizophrenia Research from the Brain and Behavior Research Foundation. The Maltz award is considered one of the top awards in the field of psychiatric disorders.

Tuesday, February 07, 2017
University of Maryland School of Medicine Researchers Find Novel Chemical Switch That May Help Decrease Crucial Symptoms of Schizophrenia
A new study by University of Maryland School of Medicine researchers has found that in mice, adjusting levels of a compound called kynurenic acid can have significant effects on schizophrenia-like behavior. The study appeared in the latest issue of the journal Biological Psychiatry.
Thursday, April 14, 2016
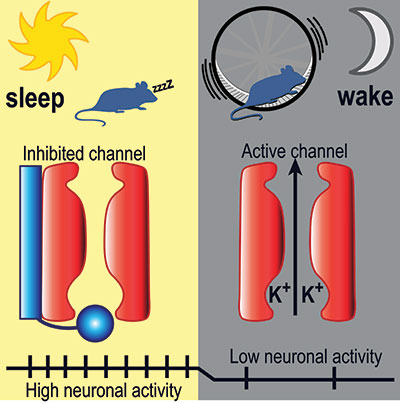
UM SOM Research Illuminates Key Aspects of How We Fall Asleep and Wake Up
Falling asleep and waking up are key transitions in everyone’s day. Millions of people have trouble with these transitions – they find it hard to fall asleep or stay asleep at night, and hard to stay awake during the day. Despite decades of research, how these transitions work – the neurobiological mechanics of our circadian rhythm – has remained largely a mystery to brain scientists.

Monday, March 14, 2016
UM SOM Sleep Experts Explore the Massive Financial Toll of Insomnia
While the benefits of a good night’s sleep can be priceless, and sleeplessness imposes significant costs on the individual and society, little is known about the financial impact of treatment for sleep-related disorders.
