May 12, 2017 | David Kohn
Study by Peixin Yang and E. Albert Reece Could Help Pave the Way to Reducing Risk for Neural Tube Defects
Researchers at the University of Maryland School of Medicine (UM SOM) have identified a gene that triggers a process leading to the formation of neural tube defects, a problem commonly found in infants of pregnant women with diabetes. This is the first time the gene has been shown to play this role; it opens up a new way to understand these defects, and may one day lead to new treatments that could prevent the problem or decrease its incidence.
The findings were published recently in the journal Nature Communications.

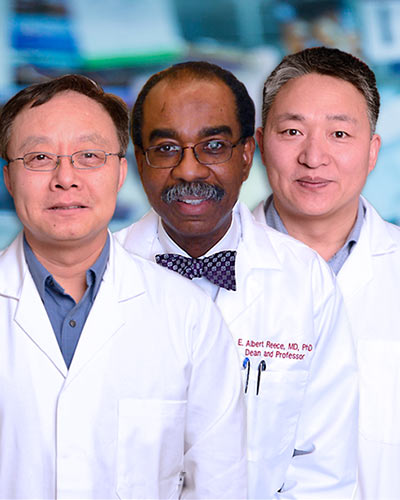
Pictured above: Peixin Yang, PhD, (third from right), E. Albert Reece, MD, PhD, MBA, and other researchers.
“This gene plays a crucial role in the process that leads to these defects,” said the study’s lead author, Peixin Yang, PhD, a Professor in the Department of Obstetrics, Gynecology and Reproductive Sciences at UM SOM. “Now that we have pinpointed the mechanism, we can begin to focus on how we can stop it from happening in humans.” Other researchers on the article include UM SOM Dean E. Albert Reece, MD, PhD, MBA, who is also the vice president for Medical Affairs, University of Maryland, and the John Z. and Akiko K. Bowers Distinguished Professor. Dean Reece has studied diabetes and pregnancy for decades, and is one of the leading experts in diabetes-induced birth defects research.
Neural tube defects (NTDs) occur when mutations accumulate in stem cells that eventually transform into the brain and the central nervous system. Under normal conditions, damaged cells are removed and replaced by healthy cells. However, in pregnancies affected by diabetes, abnormal stem cells remain in the embryo. In addition, elevated glucose causes widespread cell death. The combination of damaged stem cells and high levels of cell death in the tissues that will form the fetal brain eventually leads to birth defects, and preventing this from occurring is the ultimate goal of Dr. Yang’s work.
Even small, brief spikes in a pregnant woman’s blood glucose level can trigger diabetes-associated birth defects. Therefore, even women who monitor and control their blood sugar well are at greater risk for having a baby with NTDs than women without diabetes. In addition, this developmental process occurs very early in pregnancy, often before a woman even realizes that she is pregnant; therefore, by the time a woman confirms a pregnancy, the damage that elevated blood glucose can cause to the developing CNS might already be done.
The researchers focused on a gene called Prkca, which plays a key role in regulating autophagy, the process by which cells dispose of material they no longer need; often this material is broken or flawed in some way. In diabetes, the Prkca gene becomes overactive, and as a result autophagy is suppressed. As a result, the flawed cellular material is used to create embryonic tissue, which can lead to major birth defects.
In essence, the process is a series of dominoes. The Prkca gene triggers production of a protein called protein kinase C-alpha, or PKCalpha. PKCalpha in turn increases expression of a molecule called miR-129-2, which decreases the levels of a protein called PGC-1alpha, which encourages the destruction of flawed cells.
In an experiment using pregnant diabetic mice, Dr. Yang and his colleagues deleted this gene, which allowed autophagy to work normally. In animals in which the gene had been deleted, embryos had far fewer NTDs.
The scientists also examined whether it is possible to reduce NTDs by restoring the expression of PGC-1alpha in developing neural cells. During diabetic pregnancy, PGC-a1alpha re-activated the process of destroying flawed cells and also reduced the death of normal cells. This reduced the incidence of NTDs. Dr. Yang says that in the future it may be possible to prevent NTDs in humans by using medicines that inhibit PKCalpha or miR-129-2, or activate PGC-1alpha.
Neural tube defects are birth defects of the brain and spinal cord, and occur in the first month of pregnancy. The two most common are spina bifida and anencephaly. In the first, the fetal spinal column doesn’t close completely, which usually causes nerve damage, with some paralysis of the legs. In the latter, most of the brain and skull do not develop. Infants with this defect are usually stillborn or die soon after birth. About 10 percent of women with diabetes who are pregnant will have embryos with neural tube defects. Globally more than 300,000 pregnancies are affected by NTDs every year. In the US alone, medical and surgical costs for children born with NTDs come to more than $200 million a year. Even with high-quality preconception care, diabetic women are five times more likely to have a child with birth defects than are non-diabetic women.
“Neural tube defects remain a significant hazard for pregnant women who have diabetes,” said Dean Reece. “Women with diabetes prior to pregnancy are between three and 10 times more likely to have a child with NTDs than women without disease. This new research shines a fresh light on how we can continue to reduce this urgent problem.”
About the University of Maryland School of Medicine
Celebrating its 210th Anniversary, the University of Maryland School of Medicine was chartered in 1807 and is the first public medical school in the United States and continues today as an innovative leader in accelerating innovation and discovery in medicine. The School of Medicine is the founding school of the University of Maryland and is an integral part of the 11-campus University System of Maryland. Located on the University of Maryland’s Baltimore campus, the School of Medicine works closely with the University of Maryland Medical Center and Medical System to provide a research-intensive, academic and clinically based education. With 43 academic departments, centers and institutes and a faculty of more than 3,000 physicians and research scientists plus more than $400 million in extramural funding, the School is regarded as one of the leading biomedical research institutions in the U.S. with top-tier faculty and programs in cancer, brain science, surgery and transplantation, trauma and emergency medicine, vaccine development and human genomics, among other centers of excellence. The School is not only concerned with the health of the citizens of Maryland and the nation, but also has a global presence, with research and treatment facilities in more than 35 countries around the world. medschool.umaryland.edu/
Learn More
• Nature Communications
• Department of Obstetrics, Gynecology and Reproductive Sciences
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Related stories

Friday, March 08, 2024
People with Diabetes Who Live in Rural Areas More Likely to Develop Complications of the Disease, UM School of Medicine Study Finds
It has been well established that people who live in rural areas in the U.S. are more likely to have diabetes and experience barriers to managing their condition compared to those who live in the suburbs and cities. Now University of Maryland School of Medicine researchers have measured the devastating toll of this health disparity.
Thursday, September 09, 2021
UM School of Medicine Researchers Find Mothers’ Diabetes May Induce Premature Aging of Neural Tissue in Early Development of Fetuses, Leading to Birth Defects
More than 3 million women of birthing age in the U.S. and 60 million in the world have diabetes—a disease that occurs when blood sugar is too high. Even when controlled with insulin, and blood sugar levels are kept mostly in check, maternal diabetes can cause permanent damage to the fetus. About 300,000 to 400,000 fetuses per year from mothers with diabetes develop neural tube defects—when the tissue that eventually forms the brain and spinal cord fails to form properly—which can lead to miscarriage or profound disability.

Thursday, March 25, 2021
Longstanding UM School of Medicine Dean and Widely Recognized Academic and Institutional Leader, Dr. E. Albert Reece, Announces He Will Transition from the Deanship in 2022; His Tenure Conti
University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, a widely recognized visionary leader who elevated the UMSOM into a top-tier biomedical research and patient-focused academic center, announced that he will complete his 16-year tenure as Dean, at the end of the next academic year. He will return to the UMSOM faculty where he will lead a new Center, and continue research and teaching.

Monday, December 10, 2018
As Health Threats of the Diabetes-Obesity Epidemic Increase, Two Leading OB-GYN and Maternal-Fetal Medicine Experts Publish New Book on Diabetes and Obesity in Women
With diabetes and obesity continuing to escalate at alarming rates in the U.S., particularly among women, a new book has been published that provides the most comprehensive, expert coverage of this urgent topic to date.
Tuesday, September 12, 2017
University of Maryland School of Medicine Researchers Identify Critical Molecular Link Between Inflammation and Diabetes
A new study by researchers at the University of Maryland School of Medicine (UM SOM) has uncovered an explanation for how inflammation contributes to a key feature of diabetes, the body’s inability to metabolize glucose, a condition known as insulin resistance.
Wednesday, August 09, 2017
UM SOM Names Deputy Director of Graduate and Postdoctoral Studies for its Graduate Program in Life Sciences
Dudley K. Strickland, PhD, Associate Dean for Graduate and Postdoctoral Studies at the University of Maryland School of Medicine (UM SOM), along with UM SOM Dean E. Albert Reece, MD, PhD, MBA, announced that Peixin Yang, PhD, Professor of Obstetrics, Gynecology and Reproductive Sciences (OB-GYN), has been named Deputy Director of Graduate and Postdoctoral Studies in UM SOM’s Graduate Program in Life Sciences (GPILS).
Friday, May 12, 2017
University of Maryland School of Medicine Researchers Identify Link Between Birth Defect and Several Neurodegenerative Diseases
A new study by researchers at the University of Maryland School of Medicine (UM SOM) has found a link between some neurodegenerative diseases and a birth defect that occurs commonly in infants of women with diabetes. This is the first time this link has been identified; it may indicate a new way to understand, and perhaps treat, both the birth defects and the neurodegenerative diseases.
Wednesday, March 01, 2017
Tenth Annual “Celebrating Diversity” Dinner Supports Funding for Minority Student Scholarships
The University of Maryland School of Medicine (UM SOM) held its tenth annual “Celebrating Diversity” reception and dinner on February 25, 2017 at the Baltimore Hilton Inner Harbor. The event was attended by nearly 300 guests, who gathered to honor diversity at UM SOM, recognize those who have helped increase its diversity, and to raise money for an endowed scholarship in the name of Dean Emeritus Donald E. Wilson, MD, MACP, AGAF.
